Posters presentation by NANBIOSIS Units in CIBER-BBN ANNUAL CONFERENCE 2017
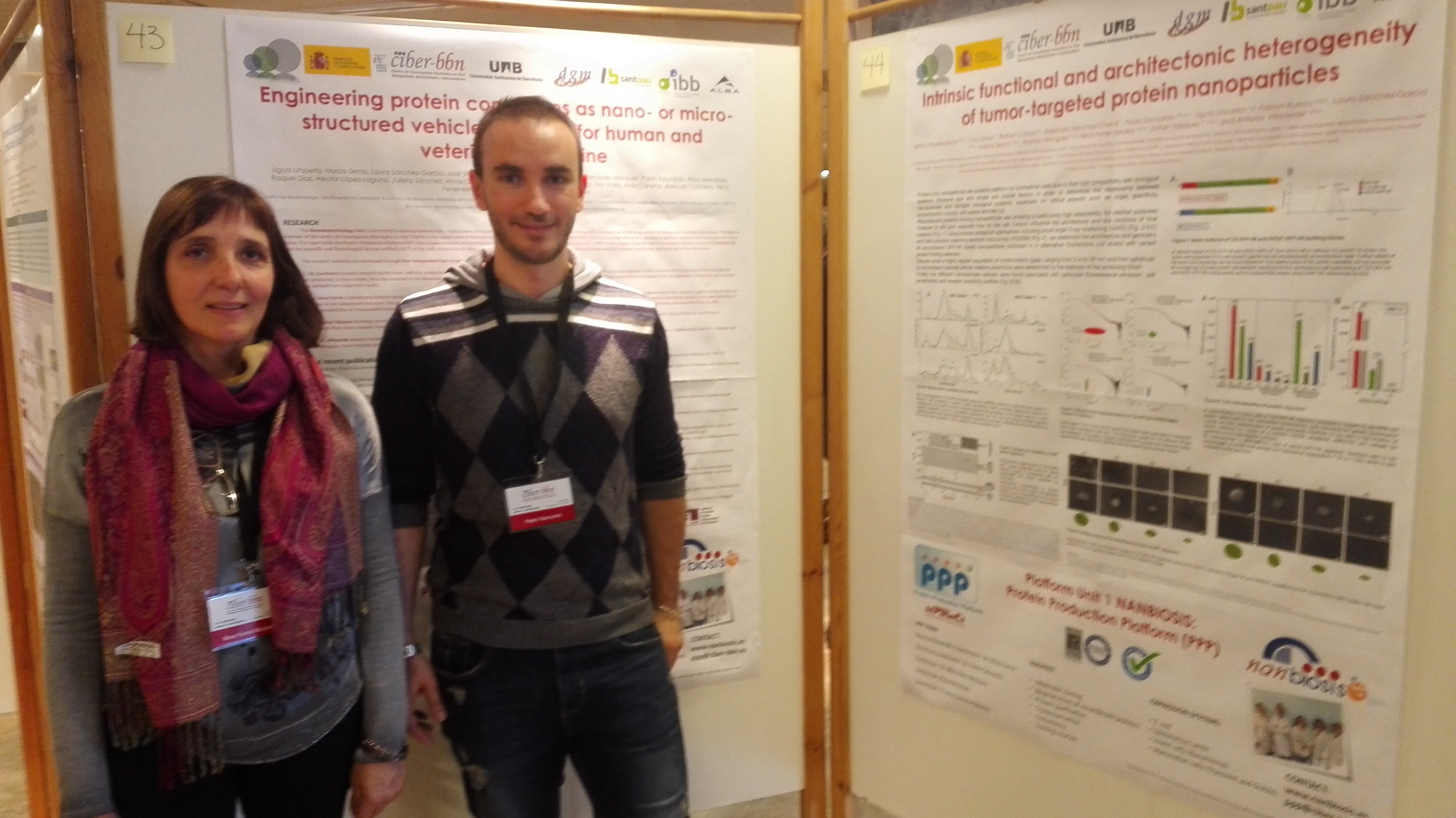
Last 13 and 14 of November, CIBER-BBN has celebrated its 11th Annual Conference in Hotel Santemar in Santander. In this conference there was a poster session with the participation of the following Units of NANBIOSIS. Special mention deserves Unit 1 with Neus Ferrer as Director and Paolo Saccardo as Coordinator (in the picture):
Posters:
U1. Protein Production Platform (PPP):
Engineering protein complexes as nano- or micro-structured vehicles or drugs for human and veterinary medicine. Ugutz Unzueta, Naroa Serna, Laura Sánchez-García, José Vicente Carratalá, Olivia Cano-Garrido, Mercedes Márquez, Paolo Saccardo, Rosa Mendoza, Raquel Díaz, Héctor, López-Laguna, Julieta Sánchez, Anna Obando, Amanda Muñoz, Andrés Cisneros, Eric Voltà, Aida Carreño, José Luis Corchero, Neus Ferrer-Miralles, Esther Vázquez, Antonio Villaverde.
Units U1. Protein Production Platform (PPP) and U18. Nanotoxicology Unit:
Intrinsic functional and architectonic heterogeneity of tumor-targeted protein nanoparticles. Mireia Pesarrodona, Eva Crosa, Rafael Cubarsi, Alejandro Sanchez-Chardi, Paolo Saccardo, Ugutz Unzueta, Fabian Rueda, Laura Sanchez-Garcia, Naroa Serna, Ramón Mangues, Neus Ferrer Miralles, Esther Vázquez, Antonio Villaverde.
Units U3. Synthesis of Peptides Unit, U6. Biomaterial Processing and Nanostructuring Unit, and U20. In Vivo Experimental Platform:
Synthesis of different length monodisperse COL-PEG-PEPTIDE to increase biodisponibility of multifunctional nanovesicles for Fabry’s desease. Edgar Cristóbal-Lecina; Daniel Pulido; Solène Passemard; Elizabet González-Mira; Jaume Veciana; Nora Ventosa; Simó Schwartz; Ibane Abasolo; Fernando Albericio and Miriam Royo.
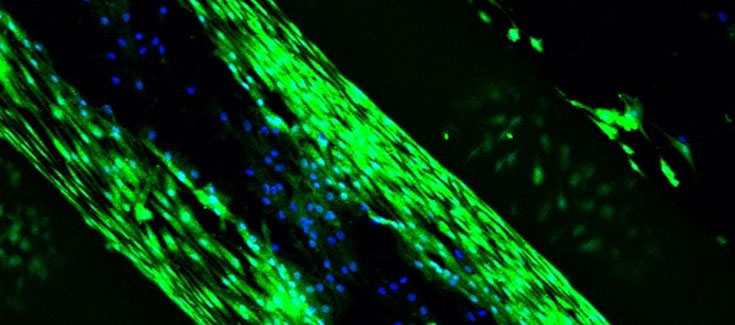
Units U13. Tissue & Scaffold Characterization Unit and U17. Confocal Microscopy Service::
Preclinical behavior of medium-chain cyanoacrylate glue with two different surgical application forms for mesh fixation in abdominal wall repair. Gemma Pascual, Bárbara Pérez-Köhler, Marta Rodríguez, Claudia Mesa-Ciller, Ángel Ortillés, Estefanía Peña, Begoña Calvo, Juan M. Bellón.
Units U27. High Performance Computing and U8. Micro – Nano Technology Unit:
Inspiration and Expiration Dynamics in Acute Emotional Stress Assessment. Javier Milagro, Eduardo Gil, Jorge M. Garzón-Rey, Jordi Aguiló, Raquel Bailón.
U5. Rapid Prototyping Unit:
Poly-DL-lactic acid films functionalized with collagen IV as carrier substrata for corneal epithelial stem cells. Ana de la Mata, Miguel Ángel Mateos-Timoneda, Teresa Nieto-Miguel, Sara Galindo, Marina López-Paniagua, Xavier Puñet, Elisabeth Engel, Margarita Calonge.
U6. Biomaterial Processing and Nanostructuring Unit:
Strategy for engineering myoglobin nano-traps for biomedical sensing technology. E. Laukhina, O. V. Sinitsyna, N. K. Davydova, V. N. Sergeev, A. Gomez, I. Ratera, C. Blázquez Bondia, J. Paradowska, X. Rodriguez, J. Guasch, Jaume Veciana.
Structure and nanomechanics of quatsome membranes. B. Gumí-Audenis, L. PasquinaLemonche, J.A. Durán, N. Grimaldi, F. Sanz, J. Veciana, I. Ratera, N. Ventosa and M.I. Giannotti
U7. Nanotechnology Unit:
Bioreceptors nanostructuration study for early detection of Alzheimer. José Marrugo, Dr. Samuel Dulay, Dr. Mònica Mir, Prof. Josep Samitier.
RGD dendrimer-based nanopatterns promote chondrogenesis and intercellular communication for cartilage regeneration. Ignasi Casanellas, Anna Lagunas, Iro Tsintzou, Yolanda Vida, Daniel Collado, Ezequiel Pérez-Inestrosa, Cristina Rodríguez, Joana Magalhães, José A. Andrades, José Becerra, Josep Samitier.
Long-range electron transfer between redox partner proteins. Anna Lagunas, Alejandra GuerraCastellano, Alba Nin-Hill, Irene Díaz-Moreno, Miguel A. De la Rosa, Josep Samitier, Carme Rovira, Pau Gorostiza.
U8. Micro – Nano Technology Unit:
Miniaturized multi-sensing platform for pH and Dissolved Oxygen monitoring in Organ-On-aChip systems. M. Zea, A. Moya, I. Gimenez, R. Villa, G. Gabriel.
Electrochemical characterization of SWCNTs based microelectrodes fabricated by inkjet printing. M. Mass, A. Moya, G. Longinotti, M. Zea, M. Muñoz, E. Ramon, L. Fraigi, R. Villa, G. Ybarra, G. Gabriel.
U9. Synthesis of Nanoparticles Unit:
In vivo imaging and local persistance of polymeric micro- and nanomaterials labelled with the near infrared dye IR820. Isabel Ortiz de Solórzano, Gracia Mendoza, Inmaculada Pintre, Sara García-Salinas, Víctor Sebastián, Vanesa Andreu, Marina Gimeno, Manuel Arruebo.
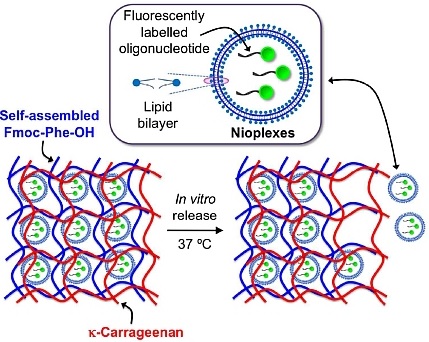
U10. Drug Formulation:
Cationic nioplexes-in-polysaccharide-based hydrogels as versatile biodegradable hybrid materials to deliver nucleic acids. Santiago Grijalvo, Adele Alagia, Gustavo Puras, Jon Zárate, Judith Mayr, José Luis Pedraz, Ramon Eritja
U12. Nanostructured liquid characterization unit:
Perfluorocarbon-loaded Nanocapsules from Nano-emulsion Templates as Microbubble Precursors for Biomedical Applications. G. Calderó, A. González, M. Monge, C. Rodríguez-Abreu, M.J.García-Celma, C. Solans.
Biodistribution study of polymeric drug-loaded nanoparticles in murine model. Marta Monge, Aurora Dols, Stephane Fourcade, Aurora Pujol, Carlos Rodríguez-Abreu, Conxita Solans.
U16. Surface Characterization and Calorimetry Unit:
Behavior and a comparative study between tantalum and titanium alloy implant surfaces against bacterial adhesion. M.A. Pacha-Olivenza, M.L. González-Martín.
Bacterial adhesion on calcium ion-modified titanium implant surfaces. M.A. Pacha Olivenza, R. Tejero, M. Delgado-Rastrollo, M.L. González-Martín.
Bioactive coatings to promote tissue regeneration and ingrowth into 3D custom-made porous titanium endoimplants (COATREG-3D). Santos-Ruiz L; Granados JF; Ruiz F; Yáñez JI; González A; Cabeza N; Vida Y; Pérez-Inestrosa E; Izquierdo-Barba I; Vallet-Regí M; Rubio J; Orgaz F; Rubio N; González ML; Peris JL; Monopoli D; Becerra J.
U17. Confocal Microscopy Service:
Subcutaneous implantation of a biodegradable apatite/agarose scaffold: biocompatibility and osteogenesis characterization in a rat model. Natalio García-Honduvilla, Gemma Pascual, Miguel A. Ortega, Alejandro Coca, Cynthia Trejo, Jesús Román, Juan Peña, María V. Cabañas, Julia Buján, and María Vallet-Regí.
U25. NMR: Biomedical Applications I:
Dual T1/T2 NCP-based novel contrast agents for brain tumor MRI: a preclinical study. Suarez, S; Arias-Ramos, N; Candiota, AP; Lorenzo, J; Ruiz-Molina, D; Arús, C; Novio, F.
Metronomic treatment in immunocompetent preclinical GL261 glioblastoma: effects of cyclophosphamide and temozolomide. Ferrer-Font, L; Arias-Ramos, N; Lope-Piedrafita, S; Julià- Sapé, M; Pumarola, M; Arús, C; Candiota, AP.
U26. NMR: Biomedical Applications II:
Gated nanodevices for innovative medical therapies. Maria Alfonso, Irene Galiana, Beatriz Lozano, Borja Diaz de Greñu, Cristina de la Torre, Andrea Bernardos, Sameh El Sayed, Daniel MuñozEspin, Miguel Rovira, José Ramón Murguía, Manuel Serrano, Ramón Martínez-Máñez.
NANOPROBE: Gated sensing materials and devices for the detection of infectious diseases and urological cancer. Ángela Ribes, Luís Pla, Sara Santiago-Felipe, Alba Loras-Monfort, M.Carmen Martínez-Bisbal, Elena Aznar, Guillermo Quintás-Soriano, José Luis Ruiz-Cerdá, María Angeles.