Researchers of NANBIOSIS U3 find activators of a possible therapeutic target for the treatment of patients with diabetes and insulin resistance
Researchers of NANBIOSIS U3: Synthesis of Peptides Unit participate in the identification of activators of of the mitochondrial protein Mitofusin 2, a possible therapeutic target for the treatment of patients with type 2 diabetes in collaboration with CIBER of Diabetes and Associated Metabolic Diseases (CIBERDEM) and the CIBER of Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN).
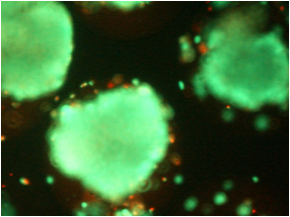
Those researchers are led by Fernando Albericio (Scientific Director of Unit 3 of NANBIOSIS) at the University of Barcelona and Antonio Zorzano en el IRB Barcelona have identified activators of the mitochondrial protein Mitofusin 2 for the treatment of type 2 diabetes. This protein is expressed at abnormally low levels in the tissues of patients with diabetes. “Thanks to the studies of phenotypic screening and validation studies in human cells, it has been possible to demonstrate the role of the protein Mitofusin 2 in the development of many of the alterations associated with diabetes”, explain those responsible for the work.
These studies have been possible thanks to the work of biologists and chemists from different CIBER areas and with experience in synthetic chemistry, molecular screening and functional analysis.
Article of reference:
Identification of New Activators of Mitochondrial Fusion Reveals a Link between Mitochondrial Morphology and Pyrimidine Metabolism. Miret-Casals L, Sebastián D, Brea J, Rico-Leo EM, Palacín M, Fernández-Salguero PM, Loza MI, Albericio F, Zorzano A. Cell Chem Biol. 2017 Dec 23. pii: S2451-9456(17)30428-2. doi: 10.1016/j.chembiol.2017.12.001.