Gold Nanoparticles Synthesized by NANBIOSIS U9 will destroy tumor cells without drugs
A CIBER-BBN team at the University of Zaragoza has developed intelligent shuttles (cell vesicles -exosomes-) to transfer nanoparticles to the interior of tumor cells and destroy them by means of heat and without drugs, following the “Trojan horse” strategy.
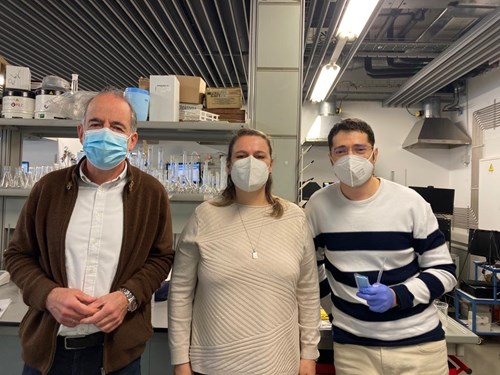
“NANBIOSIS U9, “Synthesis of Nanoparticles Unit has developed the procedure to be able to internalize gold nanoparticles, with surface plasmon in the NIR electromagnetic range, inside extracellular vesicles derived from stem cells. The synthesis of the gold nanoparticles has been produced according to the synthesis procedures of UNIT 9 of the ICTS NANBIOSIS based on the galvanic substitution reaction in the liquid phase of Co atoms by Au+3 ions, generating a hollow structure whose geometry gives gold nanoparticles unique optical properties that allow the absorption of NIR light and its conversion into heat” , explain the researchers of NANBOSIS U9 Pilar Martín-Duque, Victor Sebastián and Jesús Santamaría.
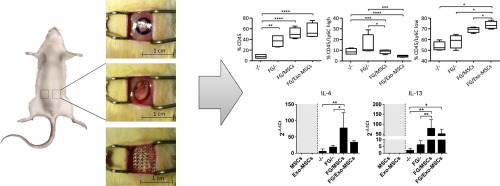
They are gold nanoparticles belonging to what is known as “plasmonic nanoparticles” that have the ability to heat up when receiving near-infrared radiation, which penetrates the body. It is, therefore, a treatment without drugs, which uses the heat generated by the particles to cause cell death around them. These particles are taken to the tumor by exosomes, having been proved efectived in animal models.
“We have managed to reduce or eliminate tumors in mice without drugs, only with the heat generated by irradiating them with a laser. In other words, we inject the exosomes with the nanoparticles into the tail of the mouse and they alone “search” for the tumor, not only in conventional models but also in multinodular ones, similar to metastatic processes”, explains Pilar Martín Duque.
For futher information:
Article of reference:
Transfer of photothermal nanoparticles using stem cell derived small extracellular vesicles for in vivo treatment of primary and multinodular tumors. María Sancho-Albero, Miguel Encinas-Giménez, Víctor Sebastián, Estela Pérez, Lluis Luján, Jesús Santamaría, Pilar Martín-Duque Journal of Extracellular Vesicles 2022 https://onlinelibrary.wiley.com/doi/full/10.1002/jev2.12193